Acquired brain injuries
Providence Health Care's services and resources for adults living with acquired brain injuries.
Overview
Acquired brain injuries (ABIs) encompass a broad spectrum of conditions affecting the brain after birth. These injuries can result from various factors. The two primary types are Traumatic brain injury (TBI) and Non-traumatic brain injury (NTBI).
- Traumatic brain injury (TBI): TBI occurs when an external force, such as a blow or jolt to the head, disrupts normal brain function. This can happen in accidents, falls, or sports-related incidents. The brain may be directly affected by the trauma, leading to a range of physical and cognitive challenges.
- Non-traumatic brain injury (NTBI): NTBI refers to brain injuries caused by internal factors like strokes, infections, tumors, or oxygen deprivation. These injuries may be more subtle but can have profound and lasting effects on cognitive function.
TBIs are more commonly associated with accidents and traumatic events, affecting millions of individuals annually. NTBIs, often related to medical conditions, also impact a substantial number of people. The prevalence of each type underscores the importance of awareness and preventive measures.
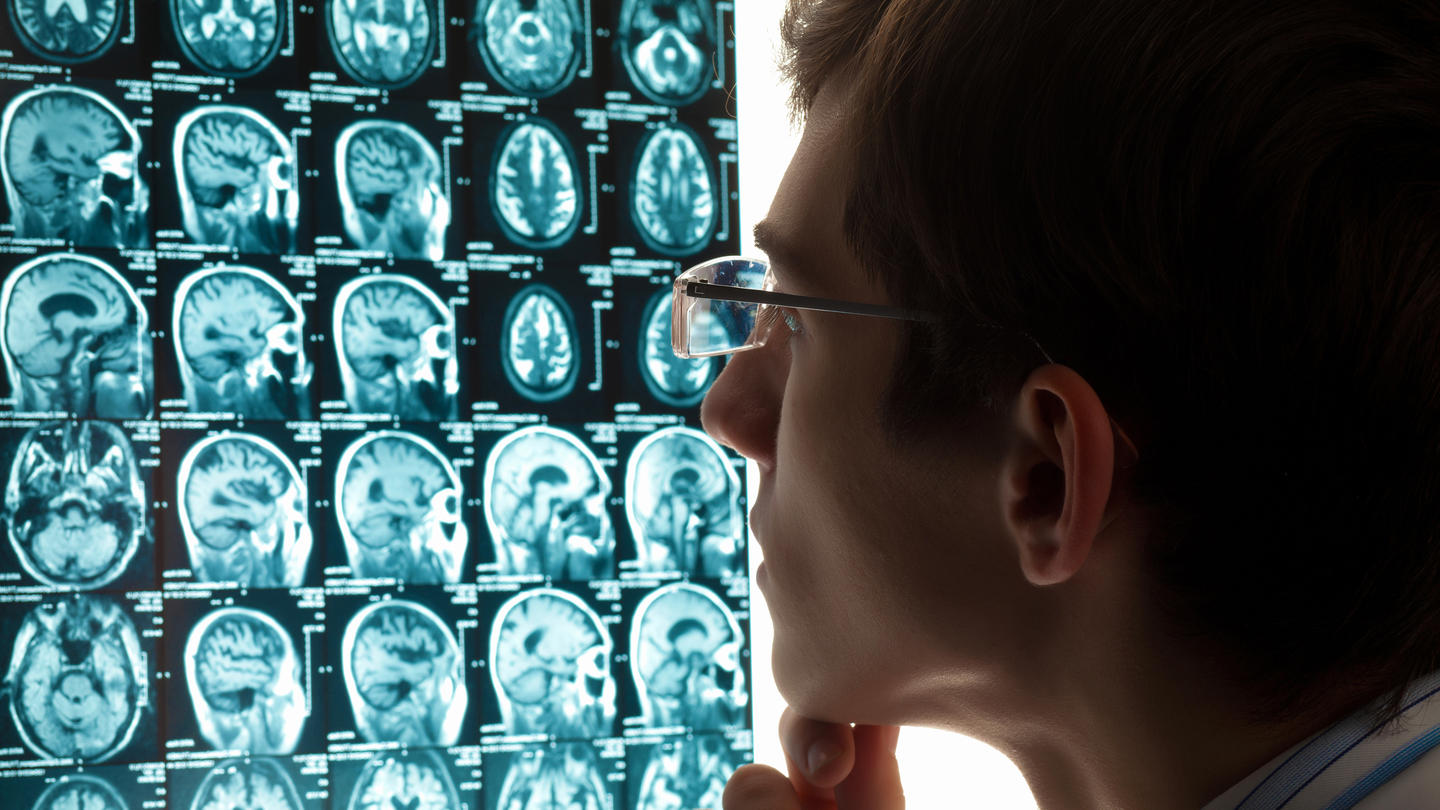
Diagnosis & testing
Diagnosing ABIs involves a careful assessment by healthcare professionals. To help diagnose an ABI, your doctor or mental health professional may use a combination of:
- Imaging tests
- Blood tests
- Neurological exams
- Reviewing patient history
Early detection or early identification allows for timely intervention and improved outcomes.
Treatment & management
While both types of ABIs impact brain function, their causes and manifestations differ significantly. TBIs result from external force, while NTBIs stem from internal factors. Understanding these differences helps tailor interventions for optimal outcomes.
Managing a TBI involves a multidisciplinary approach, including rehabilitation, medication, and cognitive therapy.
Addressing NTBIs involves treating the underlying cause. This may include surgery, medication, rehabilitation, or a combination of these.
Your journey is unique, and finding the right combination of treatments may take time. Our treatment approach is embedded in the values of the Recovery Model Philosophy. The Recovery Model is based on mutual respect and trust. We work to build positive relationships and partnerships between you and our staff and care providers. The focus is to instill hope and inspire you to work toward your own personal goals and enhance quality of life. Support from family and caregivers plays a crucial role in the recovery journey.
Hospital (inpatient) treatment
For people whose symptoms require inpatient hospitalization, we offer inpatient care at a variety of locations. We provide collaborative, evidence-based treatment that integrates primary and mental health care, using both psychotherapy and medication to stabilize symptoms.
There are four general inpatient mental health units at St. Paul’s Hospital with a total of 60 beds. Adults with mental health concerns and addictions are assessed and treated here and then discharged back to their communities.
Alder Neuropsychiatry Long Term Stabilization Unit – St. Vincent’s: Langara
Alder provides a range of specialized services to meet the needs of adults with complex neurological disorders/brain injuries and psychiatric illness. These needs prevent them from living successfully in community settings.
This regional program, for clients of Fraser Health Authority and Vancouver Coastal Health Authority, treats patients with an established neuropsychiatric diagnosis and treatment plan in place. The program is located at St. Vincent's: Langara in a specialized unit serving 20 adult mental health clients. Alder serves clients between the ages of 18 – 64 years. The length of stay ranges from 18 months to a length determined by the individual’s specific needs.
Clinics that treat acquired brain injuries
Support services
Support for Indigenous Peoples
The Indigenous Wellness Liaison Team is here to support your health journey. Team members offer cultural support and healthcare advocacy. Learn more below or call them at 604-682-2344,62937 or email IWL@providencehealth.bc.ca.
Education & resources
Patient-centred help, resources and education about ABIs come from many sources. Some of them listed here are supplied by Providence Health Care, but other useful resources about ABIs are available from the community and from online supports.
Useful resources
Patient communities
Many adults living with acquired brain injuries find it helpful to join online communities of other people with the same or similar condition. Providence Health Care does not and cannot endorse these communities. Rather, we are providing these links as resources of note for you to consider.
Community supports
There are a number of Canadian and U.S. resources for people living with ABIs.
Clinical trials & research
Advances in treatments are all thanks to medical research. While participating in research is a decision you should make for yourself in consultation with your care team, there is much activity in this area so please ask us about our research programs if you’re interested.
By taking part in research, you can help us all learn more about advancing health outcomes and find better ways to help people live and thrive. While you cannot assume benefit to yourself, your participation can make a difference in improving care for future patients.
The following clinical trials are currently enrolling volunteers. Please ask your care team for more information or contact the research team listed on each study or trial. For other information about research at Providence Health Care, please visit Providence Research.
Medical & professional referrals
Referrals to Alder are made through a centralized intake process in collaboration with Providence Health Care, Vancouver Coastal Health, and Fraser Health Authority.
Fraser Health Resource and Systems Leader
News & stories
Last reviewed: February 9, 2024

